If you’re trying to conceive, you’ve probably done just about everything you can to get pregnant.
- Expensive fertility monitor? Check.
- Tantric yoga? Check.
- Acupuncture? Check.
If you’ve made all the healthy lifestyle changes but nothing seems to be working, it may be time to consider your sleep. Some evidence suggests that there’s a link between sleep and fertility for both men and women, and it could be more important than you think.
Let’s dive into the research for all the details and look at some tips on healthy sleep hygiene for fertility.
Sleep Deprivation and Infertility:
Is There Overlap?
I speak from personal experience when I say that infertility is one of the most lonely and painful seasons. I probably took hundreds of pregnancy tests during the time I was struggling to get pregnant, and each time I saw the “negative” result it felt like a dagger in my heart.
I lost a lot of sleep during that time thanks to stress and anxiety, and if you’re struggling to conceive too, I’m sure you can relate. In some ways, it becomes a chicken and egg scenario. Maybe you were sleeping fine before you started this journey, but now that could be the very thing holding you back.
Research on sleep and infertility is still very new. Over 72 million women face infertility worldwide, and in many cases the exact cause is unknown. Unfortunately, the relationship between sleep and fertility is complicated because there are so many factors that come into play.
Given the fact that sleep is so crucial to overall health and emotional well-being, it’s not surprising that it plays a role in our ability to conceive too. Let’s start by taking a look at why sleep is so important for our bodies and minds.
The Role of Sleep
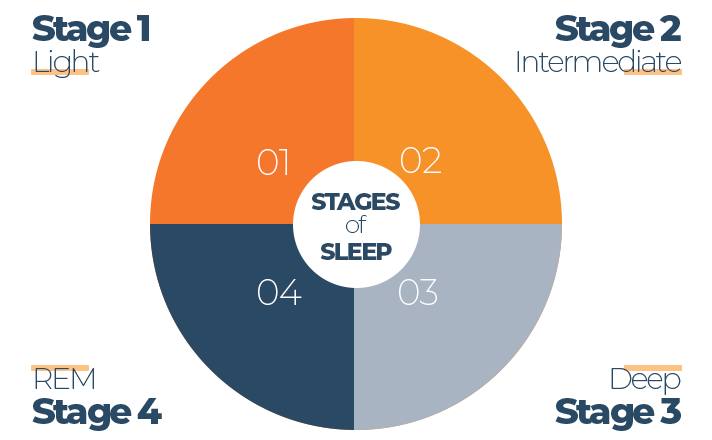
Humans spend approximately one-third of our lives sleeping, but have you ever wondered what’s happening in your body while you’re off in dreamland? There are four stages of sleep that we cycle in and out of throughout the night. Three are NREM (non-rapid eye movement) and one is REM (rapid eye movement).
Each stage is important and anything that reduces overall sleep or the time spent in one of these stages can impact health. Just like there isn’t one single cause of infertility, there isn’t one single function of sleep. Instead, sleep plays a crucial role in nearly every system of the body.
During lighter stages, the brain is working hard to consolidate information into short and long-term memories. Missing out on these stages could impact learning, memory, information processing, and so much more.
Deep sleep is when scientists believe the body works on tissue repair and new cell growth. Daily life can put a lot of stress on the body, so this stage is when the body works hard to catch up on repairs and maintenance that it can’t do during the day. Deep sleep is kind of like getting your car serviced – oils are topped up, loose threads and bolts are tightened, and all the clutter and debris are cleared away.
Some of the other functions of sleep include:
Brain Function
- Adequate sleep plays a role in decision making, information processing, memory consolidation, forming new pathways, improving attention, and creativity.
- Inadequate rest is linked to emotional instability, poor coping, anxiety, depression, and other mental illnesses.
Memory
- Sleeping and dreaming are how the brain processes memories and stores them based on the information it receives during the day.
- While we are asleep, the brain is also clearing out toxins that build up daily – including beta-amyloid, a protein associated with Alzheimer’s disease.
Physical Health
- Sleep plays a role in healing and repairing cells, regulating hormones, balancing blood sugar, growth and development, muscle building and repair, and immune function.
- Inadequate rest has been linked to all sorts of health problems including cardiovascular disease, diabetes, frequent illness, stroke, cancer, and more.
As you can see, when the body is deprived of sleep, the effects are ubiquitous. But how does that factor into the ability to conceive? Let’s take a deeper look at some of the known causes of infertility.
What Causes Infertility?
What Causes Infertility?
The American Society for Reproductive Medicine defines infertility as “the failure to achieve a successful pregnancy after 12 months or more of appropriate, timed unprotected intercourse or therapeutic donor insemination.” In some cases, medical history or certain physical findings may warrant earlier evaluation and treatment. In women over age 35, treatment is started after 6 months instead of 12.
If you’ve been trying to conceive for some time, you’ve likely already received a referral to a physician that specializes in fertility. I remember the first appointment my husband and I went to and how overwhelming it was to hear about all of the different factors that could be causing our issues.
In most cases, it takes a lot of detective work to pinpoint the exact cause. Even if they do discover something such as a failure to ovulate, they may never be able to tell you why it started happening in the first place.
According to research, infertility may be organic – the result of something physical such as blocked tubes or problems with ovulation, iatrogenic – the adverse effect of another medical condition or treatment, or lifestyle-related – poor nutrition, weight, drugs, and alcohol.
The World Health Organization task force on the Diagnosis and Treatment of Infertility classifies the prevalence rates of infertility into the following categories:
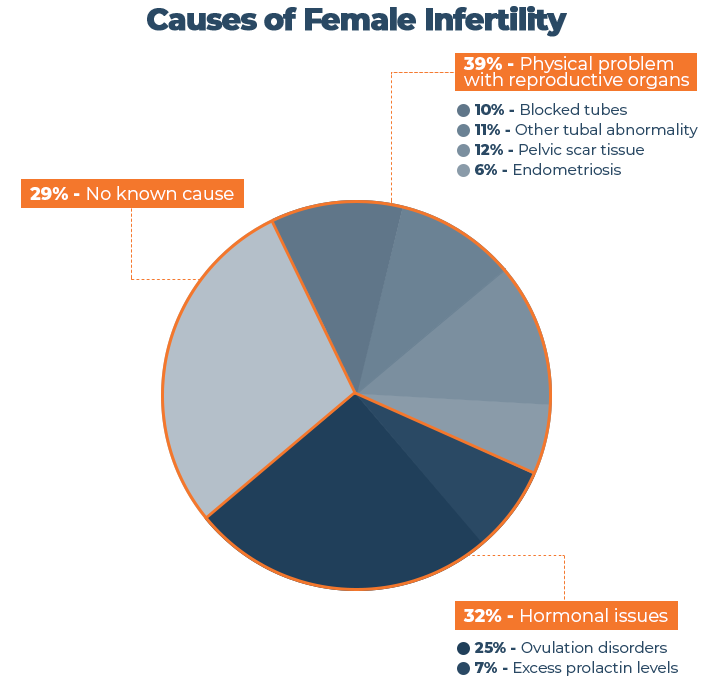
Source: “Sleep, Sleep Disturbance and Fertility in Women” – National Center for Biotechnology Information [1]
Now that we know some of the major causes, we can move on to looking more closely at the process of conception.
Conception: It’s More Complicated
Than We Think
It all starts with a little innocent flirting, a bottle of wine, and then eventually the egg and sperm meet. Seems simple, right? Wrong. The process of getting pregnant is a lot more complicated than it sounds.
Not only does it take two people to conceive, but both people have to be healthy and have properly functioning reproductive systems for the process to go smoothly. Then, there’s timing.
While men can technically get a woman pregnant any day, any time, with women, there’s a very short ‘fertile window’ of opportunity. This ‘fertile window’ refers to the days in a woman’s menstrual cycle when pregnancy is possible. For most women, there is a six-day window which includes the day an egg is released from the ovary (ovulation) and the five days beforehand.
What this means is that there are really only six days out of the entire month that women can become pregnant. It’s a wonder that humankind has been able to reproduce and experience the level of population growth that we have!
Timing isn’t the only factor for fertility. Both men and women have many other variables that must be properly functioning for conception to occur.
Male Fertility: Step One in the Investigation
Let’s start with men. Males have it slightly easier in this department because they don’t have a monthly cycle to worry about and also aren’t the ones responsible for growing babies. In fact, their role in the entire process comes down to one single job – provide healthy sperm.
People rarely think of fertility issues being caused by men, but in over one-third of couples struggling with infertility, that’s the case. According to Mayo Clinic, “Male infertility is due to low sperm production, abnormal sperm function or blockages that prevent the delivery of sperm. Illnesses, injuries, chronic health problems, lifestyle choices and other factors can play a role in causing male infertility.”
In order to get a woman pregnant, men need to produce healthy sperm (strong and fast swimmers), they need to produce enough sperm (around 40 million or more per ejaculate is ideal), and they need to be able to transport the sperm efficiently (from the testicles to be mixed with semen, then ejaculated out of the penis).
There are many different physical requirements for this whole process to go smoothly as well. Healthy sperm require healthy hormones. The penis and testicles must be healthy enough to produce sperm, maintain an erection, and ejaculate that sperm via semen.
Once the sperm make it into the vagina, they have to be strong enough to swim up through the cervix and uterus into the fallopian tubes where they can begin looking for an egg. Only the strongest swimmers make it, and they have just six days to find an egg before they die. Talk about survival of the fittest!
Female Fertility: Why Timing is Everything
There’s a lot more at stake when it comes to females and fertility. We already discussed the limited window of opportunity, but there are many other factors before and after sex that can affect conception.
Around the age of 12, most females begin menstruating and the passage from childhood into womanhood begins. The monthly cycle involves four phases: the follicular phase, the ovulatory phase, the luteal phase, and the menstrual phase. The average length is 28 days, although if you surveyed a room full of women, you’d find that some have cycles that are shorter and others much longer.
The main hormones involved in this process are follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and progesterone.
The follicular phase technically begins the first day of your period when the hypothalamus sends a signal to your pituitary gland to release FSH, stimulating your ovaries to produce 5-20 follicles. So while you’re eating chocolate and popping Midol to deal with your horrible cramps, your body is already in baby mode again.
Each of these tiny follicles contains an immature egg, but only the healthiest one will mature and the others will be reabsorbed into your body. As the follicle begins to mature, estrogen levels surge to thicken the lining of the uterus and trigger the release of LH from the pituitary gland.
This starts the ovulatory phase, which is when the ovary releases the mature egg to make its journey down the fallopian tube towards the uterus. This is the only time in the whole cycle when you can get pregnant. Two signs to look for during ovulation are an increase in basal body temperature and thick discharge with the same texture as egg whites.
The egg only has about 24 hours to be fertilized by sperm, or it dies. However, because sperm can survive for up to 5 days, there is that 6-day ‘fertility window’ leading up to ovulation.
The luteal phase is when the follicle that released the egg becomes the corpus luteum, releasing estrogen and progesterone to thicken the uterus lining further in preparation for implantation of the fertilized egg. If no egg is implanted, the corpus luteum shrinks, hormone levels drop, and the uterus lining is shed – a.k.a. the menstrual phase.
Since this is such an intricate process that requires hormones and multiple organs to be working together, there are many more things that can go wrong. Blocked tubes, irregular cycles, hormone imbalance, ovarian cysts, fibroids, and so much more. You can see why a healthy lifestyle is crucial for this process to run smoothly.
Poor Sleep’s Effect on Women
The Centers for Disease and Control (CDC) estimates that more than one-third of Americans aren’t getting the minimum of 7 hours of sleep at night that we all need.
For some women, regular shut-eye isn’t an option because of life demands like shift work, irregular schedules, travel across time zones, or a sleep disorder. Or, maybe you were one of the few that did manage to prioritize sleep prior to your journey with infertility, but now you find yourself tossing and turning just worrying about the whole process.
Higher Stress
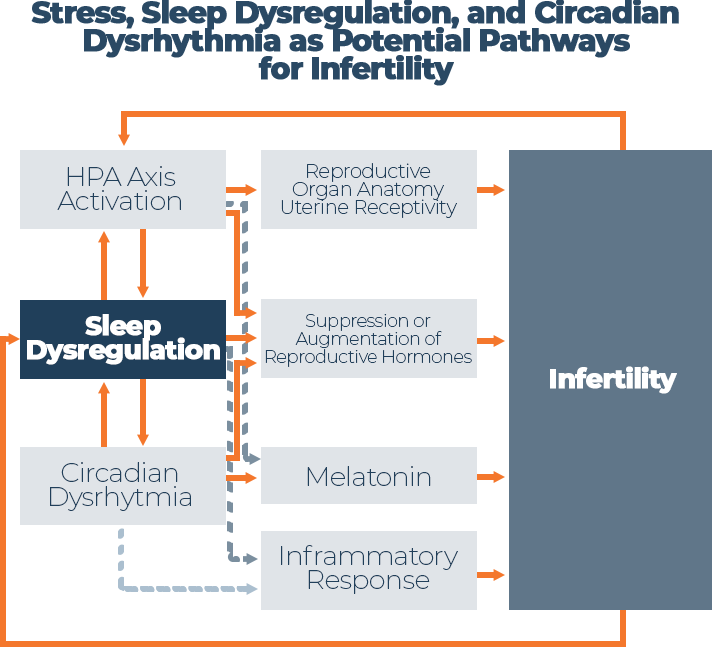
Infertility can cause a lot of stress, stress can get in the way of sleep, and too little sleep can disrupt hormones, making it harder to get pregnant. It’s a vicious cycle, but one that many women face.
One of the ways that stress affects fertility is through something called the hypothalamic-pituitary-adrenal (HPA) axis, which is partially responsible for controlling reproductive hormones, follicle development, and the menstrual cycle. Not only is HPA axis activation linked to problems with fertility, but it has also been identified as a trigger for sleep dysfunction.
Read More: Stress and Sleep
Source: “Sleep, Sleep Disturbance and Fertility in Women” – National Center for Biotechnology Information [1]
Stress hormones (adrenalin, noradrenaline, and dopamine) and the HPA axis interact with reproductive hormones which can disrupt normal ovulatory cycles. Scientists have discovered that one of the impacts of stress is altered progesterone secretion, increasing the risk of miscarriage.
Stress has also been shown to increase melatonin levels, a hormone that plays an important role in regulating the sleep-wake cycle and is also linked to reproduction. For example, increased melatonin has been linked to altered ovulation, reproductive hormone suppression, and amenorrhea (lack of menstruation).
Scientists believe that there may also be an evolutionary link between stress and fertility. Stress elicits a “fight-or-flight” response which causes many changes in the body, including altering reproduction. From a biological standpoint, if you are in a heightened state of stress (perhaps a lion is chasing you), now is not the time for growing a baby. Unfortunately, the body can’t tell the difference between stress at work and stress from something life-threatening – all it knows is “I’m in stress mode, so turn the baby-making machine off.”
In summary, stress has the potential to impair fertility along every step of the way. It can disrupt regular menstruation, ovulation, implantation, and even placental growth and development. What’s more, it can keep you awake all night, disrupting your sleep-wake cycle, which can cause lots of detrimental changes that we will explore next.
Sleep Cycle
The circadian rhythm is the body’s internal clock that relies on exposure to sunlight to regulate the sleep-wake cycle. When this cycle is disrupted, it can significantly alter fertility. Most of the research in this area has been done on shift work since many women have jobs that require them to work odd hours.
According to Megan M. Mahoney, Associate Professor of Psychology and Comparative Sciences at the University of Illinois, “Alterations or disruptions of biological rhythms, as commonly occurs in shift work, jet lag, sleep deprivation, or clock gene knock out models, are linked to significant disruptions in reproductive function. These impairments include altered hormonal secretion patterns, reduced conception rates, increased miscarriage rates and an increased risk of breast cancer.”
Nursing is one profession that is predominantly female and requires shift work, with many schedules alternating between 12-hour day shifts and night shifts. In one study of female nurses, 53% reported changes in their menstrual cycles when working shift work. Many other studies have discovered that shift work disrupts the circadian rhythm, altering melatonin levels, triggering inflammation, and hindering fertility by influencing reproductive hormones.
Another way that circadian rhythm disturbance may impair reproduction is through increased inflammation and inflammatory markers, such as CRP. A study looking at shift workers found that circadian misalignment may increase the risk of diabetes and increase inflammation in the body. Inflammation has also been linked to endometriosis, the painful growth of tissue outside the uterus that has been identified as a factor in infertility.
Circadian rhythm disruptions can also lead to insulin resistance, which is implicated in the development of polycystic ovarian syndrome (PCOS), another common cause of infertility. There is evidence that insulin resistance also increases the risk of pregnancy complications, diabetes, and cardiovascular disease in those with PCOS.
Weight
Insulin resistance and PCOS both have ties to obesity, which is also a factor when it comes to sleep and fertility. There’s a lot of growing research linking poor sleep to increased weight gain and obesity, but obesity can also hinder the body from getting proper sleep. Talk about another vicious cycle!
Obese women frequently have disturbances in the HPA axis, suffer from irregular menstrual cycles, and have excess levels of certain sex hormones. Abundant fat tissue can act like an endocrine organ, secreting hormones that contribute to insulin resistance, inflammation, and problems with reproductive egg development. Obesity has also been linked to complications including delayed conception, increased miscarriage, and poor outcome of fertility treatments.
One hormone that is produced excessively in obesity is androgen. This hormone is also tied to an increased risk of PCOS and its accompanying poor outcomes in fertility. Interestingly, obese men also suffer from poor fertility due to changes in hormone levels and increased scrotal temperatures.
Read More: Obesity and Sleep
Hormones
One thing that is clear throughout all of the research is that too little shut eye can wreak havoc on hormones. Have you ever wondered why you get the munchies at midnight, feel overly emotional when you’re not sleeping, or skip a period when your body isn’t getting the rest it needs? That’s because hormones regulate nearly every process in the body, including appetite, blood sugar, emotions, and reproduction.
The relationship between sleep disturbance and hormone levels is still not completely understood, and greater research is needed in this area. However, we do know that many hormones that are involved in conception and pregnancy operate on a circadian rhythm with increased concentrations at night. When sleep is diminished, these hormones aren’t released at optimal levels and this could be one reason why hormone levels in women struggling with infertility are often out of balance.
For example, FSH and LH are two female reproductive hormones. Both high and low levels of these hormones have been linked to infertility, and they both are also influenced by sleep. One study found that FSH levels were 20% lower in women who slept less than 8 hours per night compared to those that clocked more than 8 hours, even after controlling for age and BMI.
Menstruation
If you’ve ever had a period (and I assume you have if you’re reading this article), you know how hard it can be to sleep during your period. Between PMS, cramps, headaches, and other dreaded symptoms, falling asleep can seem like an impossible task. In fact, many women report sleep disturbances during menstruation even when they aren’t experiencing pain.
Just like during pregnancy, hormone fluctuations may be the reason why so many women struggle to get shut-eye during their monthly period.
Circadian rhythm disruption has been tied to disturbances in menstrual function. Once again, most of the research has focused on female shift workers since they are more prone to alternations in circadian rhythm. Compared to non-shift workers, female shift workers are more likely to report irregular and longer menstrual cycles.
Sleep Disorders
Sleep disorders can be caused by a number of factors, some psychological, and some physical. Many involve the same hormone disruption and circadian rhythm disturbances that have been implicated in struggles with reproduction. Chronic insomnia has been found to increase stress hormones, including cortisol, and as we talked about earlier – increased stress can make it harder to get pregnant and maintain a healthy pregnancy.
One study in Taiwan looked at data on 16,718 women diagnosed with sleep disorders between 2000 and 2010 and a comparison group of 33,436 similar women without sleep problems. They discovered that after they accounted for age and other health issues, the women with sleep disorders were 3.7 times more likely to experience infertility.
Another disorder that affects 11% of women is obstructive sleep apnea (OSA). This condition causes pauses in breathing that can severely limit oxygen and results in a whole host of health problems, including difficulty with conception. Women with OSA are also more likely to be obese and have PCOS.
The research on OSA and fertility is still new, but some evidence suggests it may increase the risk of miscarriage and that pregnancy itself may increase the risk of developing OSA or a worsening of symptoms.
If you are having trouble with sleep apnea, take a look at our list of best mattresses for sleep apnea.
What About Men?
It appears that men aren’t off the hook when it comes to sleep and fertility. In males, clocking too little or too much sleep may impact things like hormone levels, sperm count, and the ability to maintain an erection. A study at Boston University of Public Health looked at 790 couples and discovered that men who slept less than 6 hours or more than 9 hours had a 42% reduced chance of conception.
Lower Sperm Count
Remember how men need plenty of strong and healthy swimmers to fertilize an egg? A reduced sperm count is anything less than 15 million sperm per mL of semen, but the quality is also a factor. Semen quality is a measure of the shape of sperm and their motility (the ability to move forward).
A 2013 study in Denmark involving 953 healthy men undergoing determination of fitness for military service discovered a link between sleep disturbances and semen quality. Men with a higher level of sleep disturbance had a 29% lower concentration of sperm and fewer normal sperm than men who averaged normal hours of rest.
This was the first study to uncover the association between sleep and sperm, but since that time, several other studies have found a similar link.
For example, one study involving 981 healthy Chinese men found that short and long sleep duration and a later bedtime decreased sperm health. In this study, they were able to uncover a partial cause with increased levels of an antibody that attacks sperm in the semen of men identified as poor sleepers.
Erectile Disfunction
According to some research, sperm isn’t the only thing that suffers in the wake of poor sleep. Scientists have uncovered a link between sleep problems in men and erectile dysfunction.
The inability to achieve or maintain an erection can make it very difficult for a couple to conceive, and cause a lot of stress. Men tend to process stress differently than women, but one thing that suffers in the wake of stress regardless of gender is sleep.
A study in Israel surveyed 3,363 men and found a strong association between those with erectile dysfunction and those suffering from moderate to severe sleep disorders. Other research has uncovered that missing out on zzz’s can lower testosterone. Another study published in 2011 by the Journal of American Medical Association discovered that after one week of sleeping less than 5 hours per night, men had 15 percent less testosterone than normal, resulting in reduced libido.
Obstructive Sleep Apnea
Earlier, we talked about how OSA can negatively impact women’s ability to get pregnant, but research shows that it has similar effects on men too. Multiple studies have found that men who have OSA secrete abnormally low levels of testosterone at night and also suffer from higher rates of erectile dysfunction.
According to an article published in the World Journal of Men’s Health, “Both the quantity and quality of sleep affect testosterone levels. Patients with OSA have less REM sleep, reduced deep sleep time, increased nighttime awakenings, sleep fragmentation, and reduced sleep efficiency, which leads to a low testosterone level.”
While up to 60% of men with OSA report struggling with erectile dysfunction, the good news is that successful treatment with CPAP therapy can bring significant improvement in this area.
Can Better Sleep Improve IVF Success?
In the wake of infertility, many couples choose to pursue in-vitro fertilization (IVF). This can be a long and painful process, requiring multiple rounds and injections of artificial hormones. The stress and hormonal fluctuations can have a severe impact on sleep, and it turns out that sleep may have an impact on IVF success too.
Only 40% of IVF cycles result in live births, yet each cycle can be costly in the funds required to pay for the treatment and in its toll on women’s health. A study in Taiwan looked at the effect on psychological distress and sleep disturbance in women undergoing IVF and found that 23% experienced poor sleep during egg retrieval and 46% at the time of embryo transfer.
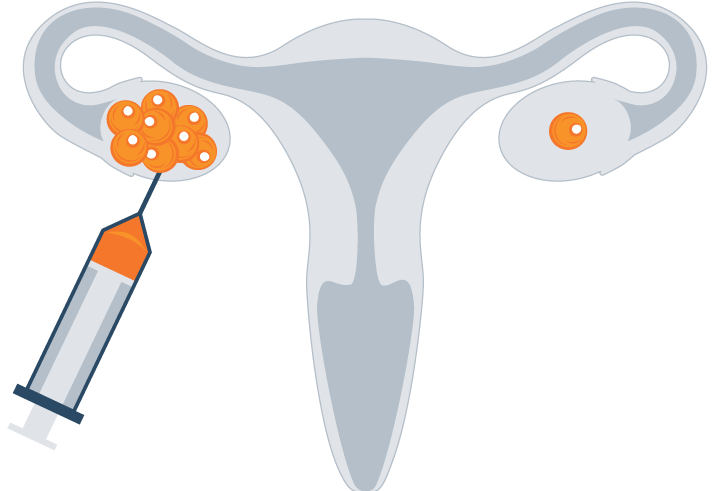
In one of the first studies of its kind, researchers looked at a small pilot sample of females undergoing IVF and found a trend with an increase in the number of eggs retrieved for every 1.5 hours of increased total sleep time.
Researchers in Japan at Hanabusa Women’s Clinic also discovered that poor quality of rest can have a negative influence on IVF. 208 women who underwent IVF were classified into one of three categories based on sleeping difficulties: no difficulty, mild difficulties, or severe difficulties.
The scientists found that the women who reported no difficulties had eggs that were 20% more likely to be fertilized, concluding that, “Good sleep patterns can be one of the important daily habits for patients to improve their response to fertility treatments and increase their chances of pregnancy.”
Another factor that may influence IVF success is the ratio of antioxidants in the body versus free radicals, a measure that is known as ‘oxidative stress.’ Without making you feel like you’re back in high school biology, we can sum up free radicals as oxygen-containing molecules that have an uneven number of electrons, allowing them to easily react with other molecules. Free radicals have the potential to cause a lot of damage in the body, but antioxidants can help by donating an electron to make them less reactive.
A lot of research has been done around oxidative stress and its negative impact on IVF. Melatonin is a hormone that plays a role in the circadian rhythm and the sleep-wake cycle but also acts as an antioxidant in the body. There is also a lot of evidence pointing to the idea that melatonin may play a larger role in human reproduction that was previously thought, acting as an antioxidant to reduce oxidative stress.
Multiple studies have been done using melatonin to improve the success of IVF treatments. Overall, the results have been very positive, although research is still in its infancy. Some of the research even found that men may benefit from melatonin with a higher percentage of viable sperm and greater sperm motility.
Questions For Your Doctor
Could melatonin be right for me?
If you’re struggling with sleep, you may be wondering if taking a melatonin supplement could help. A systematic review and meta-analysis found that melatonin is a remarkably safe antioxidant and may improve clinical pregnancy rates with no adverse effects. As we just talked about, it may even improve IVF treatments if that is something you are currently exploring too.
As with any supplement, it’s important to discuss the risks and benefits with your doctor before starting melatonin. While it does have a long history of safety, research on its use in early pregnancy is limited so it’s important to use it with caution while trying to conceive.
Find Out More: Best Melatonin Supplements
How much sleep should I be getting?
According to the UNC Fertility, 7-8 hours of sleep at night while you’re trying to conceive is ideal, increasing the chance of pregnancy by up to 25%. In fact, this is the recommended amount for all adults, but it may be especially important for women trying to get pregnant. In women undergoing IVF, getting less than 7 hours could reduce their success by as much as 15%.
If you’re struggling to fall asleep or find yourself tossing and turning all night long, speak to your doctor about how this may be impacting your ability to conceive.
Learn more: How Much Sleep Do We Really Need?
Could my medications be keeping me up?
Both prescription and over-the-counter medications can interfere with falling and staying asleep. Medications for thyroid disorders, blood pressure, headaches, colds and flus, and those for anxiety and depression are just some of the types that are known to cause disturbances.
If you suspect your medication could be causing problems, talk to your doctor about whether changing the dose or type of medication could help.
Improving Fertility With Sleep Hygiene

Take a Walk
Exercise is good for the body and can help with shut-eye too. When it comes to exercise and fertility, moderation is key. Heavy exercise can be stressful on the body, even disruption normal menstruation.
Save the marathon training for another time, and focus on fun activities that you enjoy and get the heart pumping. Also, remember to exercise earlier in the day to prevent any disruptions in falling asleep at night.
Get Some Sun
Getting some exposure to natural sunlight and vitamin D can be a great way to keep your internal clock in sync.
Regulating your circadian rhythm is important for balancing the hormones that regulate sleep and the menstrual cycle. Sunshine can also boost your mood, combatting depression and anxiety.
Shut off Gadgets at Night
There’s been a lot of talk recently about artificial blue light emitted from electronic screens and its effect on melatonin production.
The best ways to minimize exposure are to reduce screen time at least an hour before bed, use blue-light blocking glasses, and to use a screen filter to reduce blue-wave light.
Try Meditation or Acupuncture
Before turning to pills or other chemicals to help you de-stress, consider meditation and acupuncture.
Both have been shown to improve sleep without any harmful side effects. Lowering stress is also beneficial for fertility, so you’ve got nothing to lose in getting your zen on! Which one do you prefer, meditation or acupuncture?
Go Stimulant-free
We’ve all had those days where it takes a lot of caffeine to get us going and a little vino to help us unwind, but studies show that both can be harmful when it comes to our sleep.
Doctors also recommend limiting caffeine and alcohol when you’re pregnant, so it’s a good idea to start practicing reducing your consumption or at least avoiding both for several hours before bedtime.
Get Up at the Same Time
Maintaining a regular schedule for going to bed and waking up may seem trivial, but it could help to regulate your circadian rhythm.
When you go to bed and get up at the same time every day, it could help you to fall asleep faster and wake up feeling more rested.
Let Yourself Off the Hook
Stress can be one of the biggest culprits negatively impacting sleep. Infertility is stressful, but the truth is – worrying about it won’t change anything. In fact, it may even make things worse!
Instead of tossing and turning all night, wondering if there’s something new you haven’t tried, let yourself off the hook. Journaling or talking with someone you trust about your feelings may help you to let go of some of your worries and anxiety.
Consider a New Mattress
Want to spice things up? Consider getting a mattress that helps you and your partner enjoy alone time with one another.
Explore our top picks for the best mattresses for sex.
Conclusion
It’s been a decade since a fertility specialist told me that I had less than a 1% chance of ever conceiving naturally. I spent many nights stressing about the situation, which didn’t change a thing. Looking back, I wish I had just gone on a trip to Hawaii or caught up on zzz’s while I still could – because three kids later, I hardly ever sleep!
It can be challenging to prioritize rest and get your brain to shut off when you’re worried about getting pregnant. But when it comes to fertility, the science behind sleep wins again. Plus, just by spending more time in bed with your partner, you may just find you get lucky! Explore our Best Mattresses of 2024 today!

Raina Cordell
RN, RHN, Certified Health Coach
About Author
Raina Cordell is a Registered Nurse, Registered Holistic Nutritionist, and Certified Health Coach, but her true passion in life is helping others live well through her website, www.holfamily.com. Her holistic approach focuses on the whole person, honing the physical body and spiritual and emotional well-being.
Combination Sleeper
Sources and References:
[1] Sleep, Sleep Disturbance and Fertility in Women, National Center for Biotechnology Information
